Wearable AI Revolution: Seven Ways Technology Could Transform Australian General Practice
Wearable AI devices costing $800-1,200 AUD promise to address GP challenges including time constraints, diagnostic accuracy, documentation burden, and continuity of care through sophisticated medical applications.
Key Transformation Areas:
● Real-time clinical decision support providing diagnostic criteria and drug interaction alerts during consultations
● Automated clinical documentation reducing administrative time by 60-70% through AI transcription and structured note generation
● Enhanced patient monitoring enabling continuous chronic disease management between appointments with proactive intervention alerts
● Consultation quality enhancement tracking communication patterns and ensuring comprehensive preventive care discussions
Advanced Capabilities:
● Emergency response protocols displayed through smart glasses during critical situations
● Professional development feedback identifying knowledge gaps and suggesting targeted learning opportunities
● Seamless practice management integration automatically updating appointments, billing, and quality improvement metrics
Implementation Requirements: TGA approval essential for clinical devices, with careful attention to privacy compliance and professional liability considerations.
The Future of General Practice: How Wearable AI Could Revolutionise Patient Care
Imagine walking into your consultation room where your smart glasses instantly access a patient’s complete medical history, your AI pendant discreetly monitors consultation quality, and your smartwatch alerts you to critical patient data changes in real-time. This isn’t science fiction—it’s the emerging reality of general practice enhanced by wearable artificial intelligence.
As wearable AI devices become more sophisticated and medically validated, they’re positioned to address some of the most pressing challenges facing Australian GPs: time constraints, diagnostic accuracy, documentation burden, and continuity of care. With devices ranging from medical-grade smartwatches costing $800 AUD to AI-powered consultation assistants starting at $1,200 AUD, these technologies are becoming increasingly viable for modern medical practice.
Let’s explore seven key ways wearable AI could genuinely transform general practice in the near future.
1. Real-Time Clinical Decision Support
During a complex consultation with multiple presenting symptoms, your wearable AI device could provide discrete clinical decision support by analysing patient data, symptoms, and medical history in real-time. Smart glasses might display relevant diagnostic criteria, drug interactions, or evidence-based treatment guidelines without interrupting patient interaction.
These systems could flag potential red flags based on symptom combinations you might not immediately recognise, particularly valuable during busy periods when cognitive load is high. For instance, if a patient presents with seemingly unrelated symptoms, the AI might identify patterns suggesting conditions like thyroid dysfunction or autoimmune disorders.
Furthermore, these devices could provide medication dosing calculations, contraindication alerts, and allergy warnings based on the patient’s current prescription history, reducing the risk of prescribing errors whilst maintaining consultation flow.
2. Automated Clinical Documentation
Documentation burden significantly impacts GP satisfaction and patient interaction time. Wearable AI devices equipped with advanced natural language processing could automatically transcribe consultations, generating structured clinical notes that integrate seamlessly with electronic health records.
AI pendants could listen to consultations and automatically extract key clinical information—presenting complaints, examination findings, diagnoses, and treatment plans—formatting them according to standard medical documentation requirements. This technology could reduce documentation time by 60-70%, allowing more time for direct patient care.
Additionally, these systems could ensure documentation completeness by prompting for missing information, such as vital signs, allergy updates, or preventive care screenings, helping maintain comprehensive patient records whilst supporting quality improvement initiatives.
3. Enhanced Patient Monitoring and Follow-up
Wearable devices could revolutionise chronic disease management by providing continuous patient monitoring between appointments. Smartwatches worn by diabetic patients could transmit glucose trends, whilst those with hypertension could share blood pressure patterns, enabling proactive intervention before problems escalate.
Your AI system could analyse this continuous data stream, alerting you only when clinically significant changes occur. This reduces information overload whilst ensuring critical issues receive prompt attention. For example, the system might detect concerning blood pressure trends in a patient with cardiac conditions, suggesting earlier review or medication adjustment.
Moreover, these devices could facilitate personalised patient education by tracking medication adherence, lifestyle factors, and symptom patterns, enabling more targeted discussions during follow-up appointments.
4. Consultation Quality Enhancement
Maintaining consistent consultation quality whilst managing time pressures challenges even experienced GPs. Wearable AI devices could provide subtle feedback about consultation patterns, helping identify areas for improvement without being intrusive.
These systems might track consultation duration, patient engagement indicators, and communication patterns, providing aggregated feedback that helps optimise your consultation style. They could identify when you consistently run overtime with certain types of appointments, suggesting more efficient approaches or highlighting when additional time allocation might be beneficial.
Additionally, they could ensure important topics aren’t overlooked during busy periods, providing gentle reminders about preventive care discussions, medication reviews, or mental health screenings based on patient age, risk factors, and previous visit patterns.
5. Seamless Integration with Practice Management
Modern general practice involves complex coordination between clinical care, administrative tasks, and practice management requirements. Wearable AI devices could streamline these workflows by intelligently connecting clinical activities with administrative systems.
Smart devices could automatically update appointment status, trigger billing processes, and schedule follow-up care based on consultation outcomes. They might also coordinate with practice staff by sending discrete alerts about urgent results, prescription requests, or patients requiring immediate attention.
Furthermore, these systems could assist with quality improvement initiatives by automatically collecting relevant clinical indicators, patient satisfaction metrics, and practice efficiency measures, supporting continuous professional development and practice optimisation.
6. Emergency Response and Critical Alert Management
General practice occasionally involves managing medical emergencies or recognising critically unwell patients. Wearable AI devices could enhance emergency response capabilities by providing immediate access to critical protocols and facilitating rapid communication with emergency services.
During urgent situations, smart glasses could display emergency treatment protocols, medication dosages, or resuscitation guidelines whilst your hands remain free for patient care. They could also automatically alert emergency services with precise location information and preliminary patient assessment data.
Additionally, these devices could help identify deteriorating patients by monitoring subtle changes in vital signs or behaviour patterns that might not be immediately apparent during brief consultations, potentially preventing adverse outcomes through earlier intervention.
7. Professional Development and Clinical Learning
Maintaining clinical competence requires ongoing learning and reflection on practice patterns. Wearable AI devices could facilitate continuous professional development by analysing consultation patterns, identifying knowledge gaps, and suggesting targeted learning opportunities.
These systems might track diagnostic accuracy over time, providing feedback about areas where additional training could be beneficial. They could also identify emerging clinical patterns in your patient population, suggesting relevant continuing medical education opportunities or clinical updates.
Moreover, they could facilitate case-based learning by anonymously aggregating challenging cases and connecting you with relevant specialist advice or peer consultation opportunities, supporting lifelong learning within busy practice schedules.
Implementation Considerations for Australian GPs
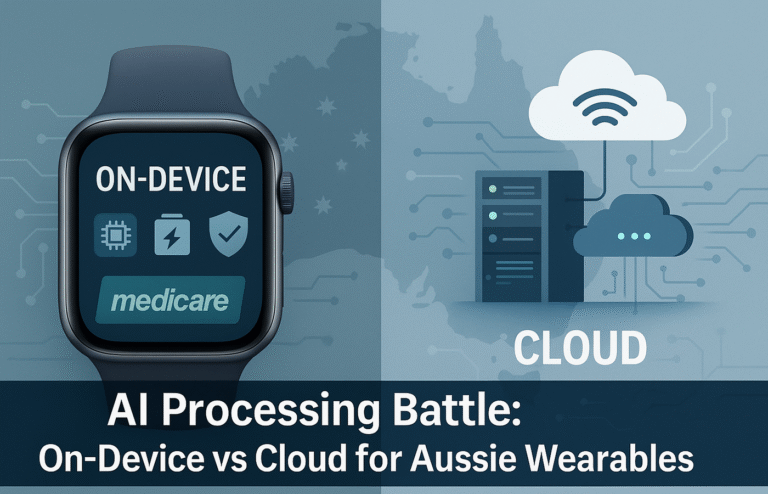
Successful integration of wearable AI into general practice requires careful attention to several key factors. Patient privacy and data security remain paramount, particularly given the sensitive nature of medical information and Australian Privacy Act requirements.
The Therapeutic Goods Administration (TGA) approval will be essential for any wearable AI devices used in clinical decision-making or patient monitoring. GPs should ensure chosen devices meet appropriate medical device standards and integrate effectively with existing practice management systems.
Training and change management will be crucial for maximising benefits whilst maintaining patient care quality. Many GPs may need support adapting to new workflows and learning to interpret AI-generated insights appropriately.
Professional and Ethical Considerations
Wearable AI in general practice raises important questions about clinical responsibility, diagnostic accountability, and the doctor-patient relationship. These tools should enhance rather than replace clinical judgment, with clear understanding of their limitations and appropriate use cases.
Professional indemnity and liability considerations will require careful evaluation, particularly regarding AI-assisted diagnostic decisions or treatment recommendations. GPs must maintain ultimate responsibility for patient care whilst leveraging technology to improve outcomes.
Patient consent and communication about AI use in consultations will become increasingly important, ensuring transparency whilst maintaining trust in the therapeutic relationship.
The Path Forward
As these technologies mature and gain regulatory approval, they promise to address many challenges facing modern general practice. Early adopters who thoughtfully implement wearable AI may find themselves better equipped to provide high-quality, efficient care whilst maintaining professional satisfaction.
The future of general practice isn’t about replacing clinical expertise with artificial intelligence—it’s about augmenting human capabilities with intelligent technology that supports better decision-making, reduces administrative burden, and enhances patient outcomes.
For Australian GPs ready to explore this technological evolution, the possibilities for improving both patient care and professional practice are genuinely transformative. These tools could help create healthcare environments where both doctors and patients benefit from more efficient, accurate, and personalised medical care.